SAN DIEGO – June 7, 2018 – Oxitope, Inc. (“Oxitope”), a privately-held biotechnology company creating diagnostics and therapeutics to treat diseases caused by maladaptive inflammation, today announced the publication of new research in the journal Nature. This publication reports that transgenic mice expressing an antibody fragment of the OxPL-targeting natural antibody E06 exhibited a decrease in systemic inflammation, atherosclerosis, aortic valve calcification, and non-alcoholic steatohepatitis (NASH) along with improved longevity over 15 months, despite extremely elevated low-density lipoprotein cholesterol (LDL-C) levels. The results demonstrate LDL-C independent effects of OxPL on these diseases, which are all age-associated inflammatory conditions that are among today’s leading causes of human morbidity and mortality.
“There has been evidence in the scientific literature, including in vitro, cell culture and epidemiology studies, showing that high levels of OxPL are associated with both acute and chronic diseases caused by maladaptive inflammatory responses. However, an in vivo demonstration of the amelioration of such effects, has not been shown until the current study,” said Joseph L. Witztum, MD, senior author and Professor of Medicine at the University of California San Diego. “This publication, and the work it embodies, represents decades of research originally initiated to elucidate the atherogenic properties of modified LDL-C and has led to a new understanding of the pathophysiological role of oxidative modifications, such as OxPL, in a variety of inflammatory disorders. It is gratifying to now see this research moving out of the laboratory and into translational activities to create diagnostic and therapeutic solutions with the potential to benefit patients.”
The study was conducted by researchers from the University of California San Diego and collaborators at Taipei Medical University; University of Eastern Finland; La Jolla Institute for Allergy and Immunology; UT Southwestern Medical Center; and the Medical University of Vienna, Center for Molecular Medicine of the Austrian Academy of Sciences. The research reported in this publication includes intellectual property invented by Drs. Witztum, Tsimikas and Que, which was part of a recent exclusive, world-wide diagnostic and therapeutic license to Oxitope of a portfolio of OxPL related intellectual property from the UC San Diego.
“These observations, combined with our license, create near and long-term opportunities to translate the findings to improve the care of patients with oxidative/inflammatory disorders which are integrally associated with chronic diseases and complications of aging,” said Alexander Martinez, President and Co-founder of Oxitope. “We are excited by the potential to create therapeutics to intervene at the intersection of accumulated damage from oxidative stress and immune system activation in order to address the highly prevalent, debilitating and often fatal inflammatory diseases people suffer from today.”
Key findings of the research published in Nature:
· OxPL are pro-inflammatory and contribute to the progression of atherosclerosis, aortic valve calcification and non-alcoholic steatohepatitis in control mice.
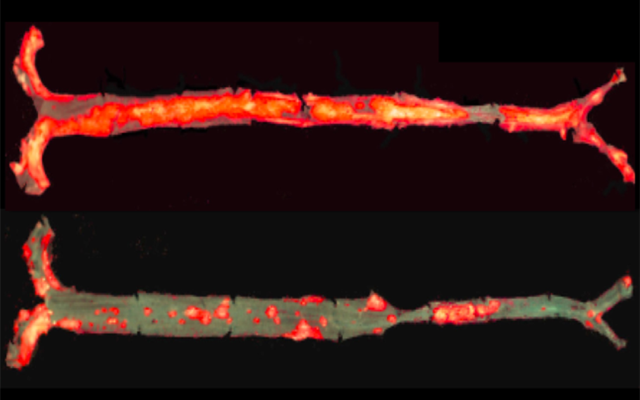
· Compared to control mice, the mice expressing the OxPL targeting antibody had 28-57% less atherosclerosis, even after one year despite continuous plasma cholesterol levels > 800 mg/dL.
· Mice expressing the OxPL targeting antibody had decreased aortic valve calcification (hardening and narrowing of the aortic valve leaflets), hepatic steatosis (fatty liver disease) and liver inflammation.
· Mice expressing the OxPL targeting antibody also had 32% less serum amyloid A, a marker of systemic inflammation, as well as reduced expression of inflammatory genes by macrophages.
· These effects contributed to the observation that targeting OxPL also prolonged the lifespan of the mice — after 15 months, 100% of the mice expressing the OxPL targeting antibody were alive, compared to 54% of the control mice.
Additional pre-clinical research using the same mouse model expressing the OxPL targeting antibody was also published today in Nature Communications, where, together with colleagues at the University of Arkansas for Medical Sciences, the authors have demonstrated that inflammatory high-fat diets induce bone loss in control mice. These effects were significantly attenuated in the mice expressing the OxPL targeting antibody due to an anabolic effect on bone formation. These findings indicate that OxPL chronically exert a restraining effect on bone formation and that age-related bone loss might be due in part to diminished ability to defend against accumulating oxidative damage, such as OxPL. Optimized versions of natural human anti-OxPL antibodies therefore, may represent a novel therapeutic approach to the prevention and treatment of osteoporosis.
Finally, in a third publication in Cardiovascular Research comparing control mice to the same mouse model expressing the OxPL targeting antibody, it was demonstrated that OxPL are generated within cardiomyocytes during ischemia-reperfusion injury, which often occurs during heart attack or procedures to open occluded arteries, and that such OxPL have detrimental effects on cardiomyocyte viability. Inactivation of OxPL in vivo resulted in a reduction of myocardial infarct size. These observations suggest opportunities for novel therapeutic options in patients suffering from myocardial infarction to preserve heart muscle function and improve long-term prognosis.
“In addition to this compelling preclinical research, our biomarker laboratory at the University of California San Diego has demonstrated in over 50 publications in humans, including prospective studies of up to 15 years, that elevated levels of OxPL measured on lipoproteins in plasma predict the development of a variety of phenotypes in cardiovascular disease and aortic stenosis,” said Sotirios (Sam) Tsimikas, MD, Professor of Medicine and Director of Vascular Medicine at the University of California San Diego, and also a co-author on the three publications. “Additionally, decreased levels of such plasma antibodies binding oxidation-specific epitopes (OSE), such as OxPL and related antigens, are associated with higher risk of cardiovascular disease. All of this work taken together supports both the diagnostic rationale for measuring the target, OxPL, to diagnose and risk stratify patients, as well as the therapeutic rationale for the development of optimized versions of evolutionary-selected and conserved natural human antibodies to OSE to treat a variety of inflammatory diseases with high unmet need despite available treatments.”
About Maladaptive Inflammation, OxPL and OxPL Targeting Medicines:
Inflammation is a protective (adaptive) response to noxious stimuli, chiefly infection or injury, intended for acute activation to restore an individual to a normal functional state. Inflammation is a high-benefit, potentially life-saving response, however, it comes at high-cost due to its ability to override normal function and cause tissue damage or even death. When inflammation is excessive or becomes chronically activated it becomes harmful (maladaptive).
The dramatic environmental changes brought about by modern human populations, including reduced microbial exposure, western diet, industrial toxins, and decreased physical activity have resulted in a population-wide burden of oxidative damage capable of sterile (in the absence of infection) activation of maladaptive inflammation. It has become widely-recognized that this maladaptive sterile inflammation is a key driver of unhealthy aging and today’s primary sources of morbidity and mortality: cardiovascular disease, cancer, obesity, metabolic disease, osteoporosis, arthritis, fatty liver disease, and neurodegeneration.
The maladaptive sterile inflammatory response can be perpetuated or in some cases initiated by OxPL. Some phospholipids, such as the molecules that make up cell membranes, or are present on lipoproteins or on apoptotic cells, are prone to modification by reactive oxygen species (ROS, also known as “free radicals”), forming OxPL. This event is particularly common in inflammatory conditions where cells in the immune system generate ROS as an antimicrobial defense mechanism, leading to generation of OxPL, which then further amplifies the inflammatory response, often noted as activation of inflammatory cells and their genes to generate inflammatory cytokines, such as interleukins. OxPL can also be primarily generated when an individual is exposed to excessive, chronic oxidative stress, the imbalance between ROS and the body’s own ability to detoxify (such as through antioxidant mechanisms) or repair oxidative damage, resulting in the recognition of OxPL by the immune system and initiation of an inflammatory response.
Existing and emerging anti-inflammatory therapeutics generally target a single, downstream molecular component of an already activated inflammatory response, relying on immunosuppression to achieve a therapeutic effect. This immunosuppression limits use in broad, preventative indications and vulnerable populations. OxPL-targeting therapies, because they are not targeting components of the immune system and are generally upstream of cytokine release, have the potential to impact proximal immune system activity in a manner that attenuates multiple inflammatory pathways. Importantly, this occurs without the immunosuppressive effects of current therapies.
About Oxitope:
Oxitope’s goal is to enable people to live long and healthy lives by preventing, halting or reversing acute and chronic diseases driven by maladaptive inflammation, which today result in progressive disability and death. To that end, Oxitope is focused on developing diagnostic and therapeutic modalities that target oxidation-specific epitopes (OSE), such as OxPL. OSE are highly pro-inflammatory and play a central role in the oxidation/inflammatory contribution of many chronic diseases. Oxitope’s initial diagnostic focus is transferring its OxPL-based diagnostic tests for use in the clinical setting where measuring OxPL has predictive value, including reclassifying up to 30% of patients with cardiovascular disease, independent of traditional risk factors. Oxitope’s initial therapeutic focus is creating medicines that selectively target OxPL in rare diseases with high unmet medical need that also serve as unique opportunities to explore the biology of targeting OxPL in broader diseases of maladaptive inflammation and aging, such as non-alcoholic steatohepatitis, arthritis, atherosclerosis, aortic stenosis, ischemia-reperfusion injury, osteoporosis, pain, and autoimmune diseases.
The company can be contacted for more information at www.oxitope.com.
Media Contact
Company Name: Oxitope, Inc.
Contact Person: Alexander Martinez, J.D.
Email: Send Email
Phone: 619-354-0725
Country: United States
Website: https://www.oxitope.com/